Abstract
Background: Traumatic and bloody lumbar punctures (TLPs and BLPs, respectively) at the diagnosis of pediatric acute lymphoblastic leukemia (ALL) impair the interpretation of central nervous system status and are associated with worse outcomes. We previously analyzed risk factors for TLP and BLP in 958 patients with ALL treated at St. Jude Children's Research Hospital (St. Jude) between 1984 and 1998. With an incidence of 19% and 5% at diagnosis, respectively, TLPs and BLPs were associated with unmodifiable and modifiable risk factors (URFs and MRFs, respectively). URFs included age less than 1 year and black race. MRFs included a platelet count (PLT) of <100 × 109/L, a less experienced practitioner, a non-dedicated procedural setting, and no sedation. Since then, preventive measures have been adopted for the first lumbar puncture (LP) at St. Jude: patients undergoing an LP ideally have a PLT of ≥100 × 109/L; the procedure is performed by the most experienced practitioner available; and we use a dedicated procedure area and general anesthesia.
Objectives: To determine the incidence and risk factors of TLPs and BLPs, defined by the presence of at least 10 and 500 red blood cells per microliter of cerebrospinal fluid, respectively, at the diagnosis of pediatric ALL after the introduction of preventive measures.
Patients and Methods: We performed a retrospective cohort study on children with newly diagnosed ALL who were consecutively enrolled on the Total XV and Total XVI protocols at St. Jude from October 2000 through March 2017. Patients who received their first LP at a center other than St. Jude or did not have a PLT within 24 hours of undergoing LP were excluded.
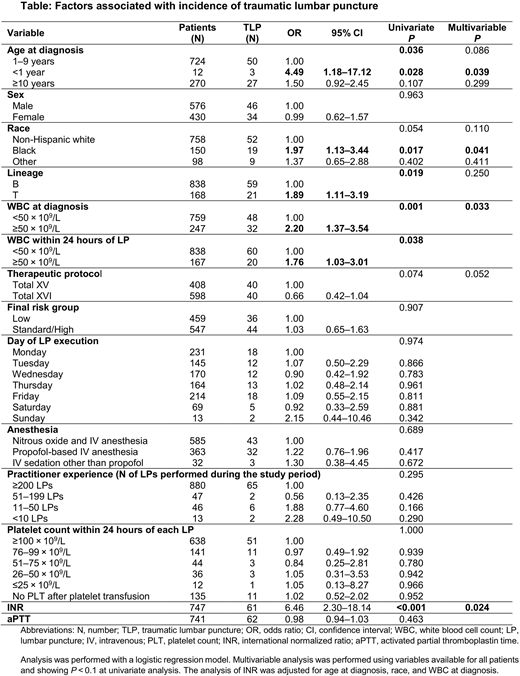
Results: A total of 1006 patients (median age, 5.68 years at diagnosis; range, 0.12 to 18.89 years) were included in our study. Of the 1006 LPs at diagnosis, 80 (7.9%) were TLPs and 15 (1.5%) were BLPs. Of the 80 TLPs, 47 (58.7%) showed leukemia blasts (vs 30.9% [286/926] of non-TLPs; P < 0.001). Of the 15 BLPs, 13 (86.7%) showed leukemia blasts (vs 32.3% [320/991] of non-BLPs; P < 0.001). Regarding the adopted preventive measures, 561 patients received a platelet transfusion within 24 hours of LP because of a low PLT, but in 135 (13.4%) of these cases, a repeat PLT was not evaluated before the procedure (see Table). Therefore, of 871 available PLTs within 24 hours of LP, 638 (73.2%) were ≥100 × 109/L and 779 (89.4%) were ≥75 × 109/L. Experienced practitioners (defined as those having performed at least 200 procedures during the study period) performed 880 (89.2%) of the 986 LPs for which practitioner information was available. General anesthesia was used in 948 (96.7%) of 980 LPs for which anesthesia information was available. All the procedures were performed in a dedicated area. We saw no significant differences in the incidence of TLP with respect to these MRFs. TLP was associated with age less than 1 year, black race, T lineage, a white blood cell count (WBC) of ≥50 × 109/L both at diagnosis and within 24 hours of LP, and a higher international normalized ratio (INR) in univariate analysis (see Table). Multivariable analysis, performed on variables available for all patients and showing P < 0.1 in univariate analysis, confirmed the association between TLP and age less than 1 year, black race, and a WBC of ≥50 × 109/L at diagnosis (see Table). INR also remained significant when adjusted for age at diagnosis, race, and WBC at diagnosis. We found no significant association between BLPs and the analyzed variables.
Conclusions: Best practices were used in almost all cases in our recent cohort, and the incidences of TLP and BLP at diagnosis decreased markedly (to 7.9% and 1.5%, respectively). This decrease can be ascribed to the adoption of preventive factors (requirements for a PLT of ≥100 × 109/L, if possible; the most experienced practitioner; general anesthesia; and a dedicated procedure area). The previous association of TLP with the URFs age less than 1 year and black race was confirmed by this study. Our analysis suggests that LPs must be performed carefully in infants and black patients, as well as in those with WBCs of ≥50 × 109/L, and that it may be preferable to delay the first LP until peripheral blood blasts disappear and the INR is normal.
Howard:BTG: Consultancy, Research Funding; Shire: Consultancy, Speakers Bureau; Jazz: Consultancy, Speakers Bureau; Sanofi: Research Funding, Speakers Bureau. Inaba:Shire: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal